Densitas Partners with RAD-AID to Advance Personalized Breast Screening in Underserved Areas Using A.I.
Feb 27, 2020Categories: General
Densitas Inc., a leading provider of A.I. technologies for digital mammography and breast screening recently partnered with RAD-AID International to establish an A.I.-based decision support program for breast health in medically underserved regions.
The aim of the partnership is to provide low-resource institutions with education, clinical support, and hands-on training so that they may adopt sustainable mammography practices that leverage practical A.I. powered applications. For breast imaging departments in participating institutions, the program is expected to help advance the quality of patient management decision-making and improve early disease detection.
We talked to Dr. Daniel Mollura, founder and CEO of RAD-AID International, to learn more about the history of the organization and the role that A.I. can play in the delivery of breast cancer screening services in underserved and low-resource regions of the world.
1. Mo Abdolell (Mo): Can you tell us about RAD-AID International?
Dr. Daniel Mollura (Dan): RAD-AID is a non-profit organization that increases and improves radiology for low-resource regions in the world, that includes low and middle-income countries, as well as medically underserved regions of high-income countries.
Our efforts include education, equipment donation and technology support for low-resource hospitals to adopt and use radiology effectively for their patients.
2. Mo: Related to that, what is RAD-AID’s mission and history, and what brought this idea to realization?
Dan: I’m a radiologist by background, and when I was doing my training at Johns Hopkins, I became very interested in the World Health Organization’s reports on the scarcity of radiology around the world. Approximately ½ to ⅔ of the world doesn’t have radiology or accessible medical imaging. So as a radiology professional, I was very interested in the impact that would have on healthcare disparities.
In turn, the absence of imaging has this ripple effect on the healthcare sector, because medical imaging is used in much of the decision making, whether it be for ultrasound in maternal infant health, or mammography for breast cancer screening, or CT scans for trauma and cancer management etc. So the absence of radiology really has a profound impact on access to care, and that led to us thinking that RAD-AID may be an effective platform for delivering more radiology to those low-resourced regions.
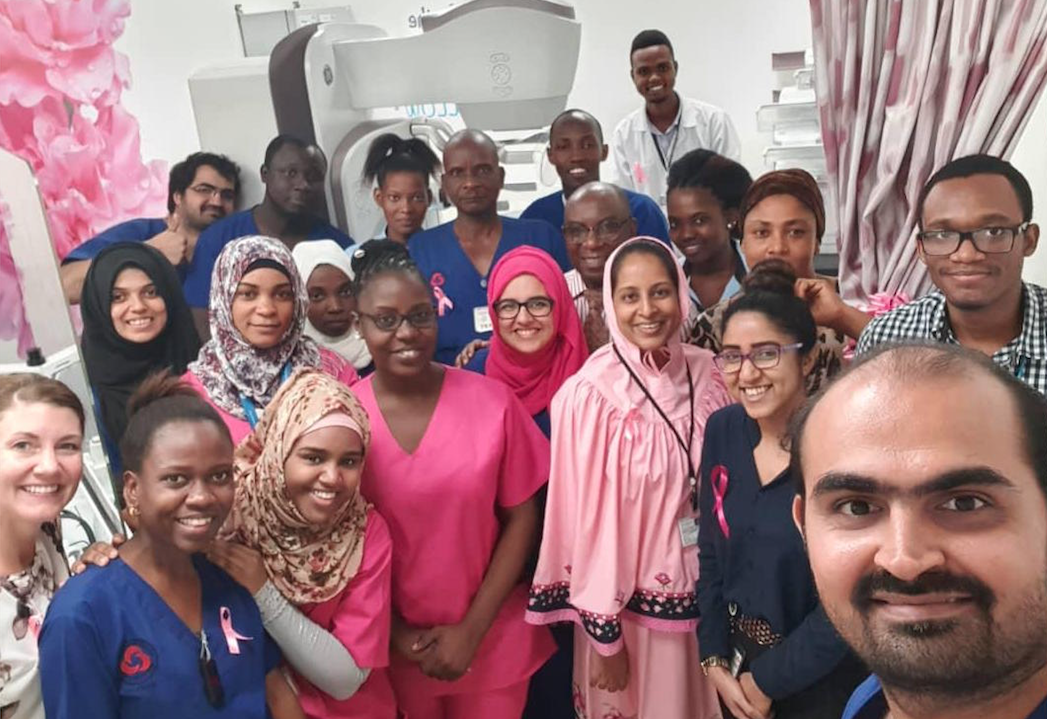
Anne-Marie Lugossy, Director of RAD-AID Tanzania, supporting mammography education for technologists, to develop breast cancer screening in Tanzania.
One of the things that’s critical here is that we knew upfront that RAD-AID itself could not create its own solutions for every single problem. Instead, RAD-AID is designed as a platform for radiologists, technologists, IT specialists, engineers, physicists, nurses, and other professionals throughout the health sector, to really channel their own creativity and own ideas for solutions into those programs. So effectively, it’s a platform for bringing people together to channel their own creative solutions to world problems.
3. Mo: How does RAD-AID select the projects that it takes on? Or do the projects select you?
Dan: The approach to developing a project starts with the Radiology-Readiness assessment. The Radiology-Readiness assessment is part of a due-diligence process for collecting information about a hospital in terms of what resources they already have and the clinical goals they have, and filling in the gaps that might exist between their existing resources and those goals.
After 12 years of doing this, we’ve gained enough visibility that most of the time now hospitals approach RAD-AID for assistance with the development of their radiology departments.
For example in Laos, Lao Friends Hospital for Children approached us in 2015 just as they were completing the construction of their hospital and wanted help to set up their radiology department. We did a Radiology-Readiness assessment and identified what was lacking and what we could provide to help them develop more radiology resources, and that led to a collaborative program to longitudinally support their radiology department development.
4. Mo: On a more personal level, what drove you to establish RAD-AID?
Dan: It was both personal and professional.
Before going into radiology and medicine I’d started a career in the Wall Street sector, and my first job was with Goldman Sachs doing investment research in the equities division. I became familiar with international finance, startups, technology companies and ways in which companies would start and try to solve a problem in the market. But ultimately I chose to leave my finance and Wall Street career behind because I wanted to make a difference in directly helping people, and thought that medicine and radiology was a better match for me.
However that love for the business side of healthcare technology innovation never left me. I wanted to combine my two career interests, now as a radiologist interested in the medical side of patient care, together with what I had learned about how organizations can form and how they can structure themselves to deliver a product or service that makes a difference.
So putting those two things together made me want to start a non-profit that could provide something very beneficial, that would harness the same kinds of strategies that the private sector would use, but do it in a way that was philanthropic, that the public sector could also benefit from.
5. Mo: Why do you think 10,000+ volunteers and industry partners are so compelled to dedicate their time and resources to the RAD-AID mission? What do you think it is about the RAD-AID mission that attracts so many people?
Dan: I think it’s the openness of the organization and the ability to channel creativity in RAD-AID that has drawn people to volunteer to make a difference. We don’t control things in a hierarchical way; our culture at RAD-AID is consensus-based and horizontal. We believe that when people have a good heart and they have a good mind and they’re solving problems, they can really work their own magic.

Patricia Ducharme, Director of RAD-AID Nursing, supporting Guyana’s nurse education program for radiology services.
And so in that sense, the organization really has an open culture of trying to bring together the very best expertise, and allowing them to address challenges in their own creative ways.
The Radiology-Readiness platform creates a road map so that things are structured, but still empowers the creativity that I think is very attractive to those with new ideas.
6. Mo: What kinds of disparities have you observed in breast cancer screening globally?
Dan: Access to breast cancer screening is extremely low throughout the world, especially in low and middle-income countries. So for example, five-year survival rates for breast cancer in Canada and the United States are somewhere close to 90%, while most rates in Africa are somewhere between 15-50%.
Now that is a multi-factorial outcome, because some of it is education, some of it is economics, and some of it is the availability of medical infrastructure. But a large part of that is due to early detection. We do know that in high-income countries and advanced healthcare sectors, access to early detection modalities such as mammography is a vital piece of making sure that women can survive breast cancer.
So what we’re seeing is multiple reasons for poor access to breast cancer screening. The two key reasons are the lack of mammography equipment and the lack of breast radiologists who can interpret mammograms, and radiological technologists who can acquire the mammograms. And then, even if you do have those elements, you also need a referral network for further workup, diagnosis and treatment. So there are multiple layers to the breast cancer pipeline of care, but the access to good breast cancer screening is really absent in most of the world.

Dr. Alice Chong, Associate Director of RAD-AID Breast Imaging in Tanzania helping breast cancer screening and radiology education in Tanzania.
I’ll give one example. Kenya has about 4-5 million women that need annual mammography. But there are only 3 fellowship-trained breast imagers in Kenya. So screening 4-5 million people with only a handful of specialist-trained breast radiologists is simply impossible at the moment. And this is not an isolated case. We’re seeing in numerous parts of the world similar numbers that confirm there is an insufficient number of breast radiologists to do the kind of work that would be necessary for an effective breast cancer screening program.
Mo: I would assume this is also true of radiological technologists as well.
Dan: That’s right, the number of technologists is significantly lower than what is needed to run an effective program. For example, according to some estimates, Tanzania has approximately 450 technologists for the whole country of approximately 58 million people. So there is over 75-fold difference in access to radiologic technologists on a per capita basis between the US and Tanzania. Which again, reinforces what you just said: access to technologists is going to be a critical piece of the radiology services pipeline.
7. Mo: What are the most pressing challenges faced by underserved areas in the delivery of breast cancer screening services? I think you’ve answered some of this already, but to dive a little deeper – even if they had equipment, what else do these underserved areas need beyond just having perhaps a software algorithm or a scanner or PACS system? Are there other pressing needs or disparities in these regions?
Dan: I think your question hits the nail on the head. One of the biggest struggles we have is the misconception that having the equipment is sufficient. We will often see situations where a hospital obtains a mammography unit, and then they quickly understand that having a mammography unit doesn’t suffice to provide an effective breast cancer screening program. You need a skilled technologist, you need an MD physician who knows how to interpret the image, you need a workflow for screening, and then another workflow for diagnostics, and then breast health navigation that comes from nursing to help patients plug into the next step for further workup, treatment, and follow up.
So the mammography scanner is just the tip of the iceberg, it’s just the beginning. And we often find that because it is such a large upfront capital cost to acquire a mammography unit, there is the mistaken assumption that such a significant outlay of funds is sufficient to deliver breast screening services.
So what we’re trying to do when we see mammography scanners acquired by hospitals is to work with them to design a program for breast cancer screening, where we train the technologists to produce quality mammograms, and train the MDs to interpret the mammograms. And now with newer technologies that are coming with Artificial Intelligence (A.I.) for mammography interpretation, or other characteristics of the mammography image, we’re trying to introduce those technologies as part of training to make breast cancer screening more effective.
8. Mo: This is a great segue to the next question. Can you expand a little further on the role of A.I. in RAD-AID’s mission, and more specifically in breast cancer screening?
Dan: Artificial Intelligence has a big potential role in RAD-AID’s outreach projects. We have been deploying PACS and cloud, and other software technologies in low-resource settings for the last seven years, and so we’ve gained an important set of experiences in integrating software, hardware, network and cloud solutions for low-resource hospitals.
Artificial Intelligence is the next big opportunity to make a significant impact on how these hospitals deliver quality patient care. Whether it be quality control or assessment, or workflow management, or automated diagnostic interpretation, these are all things that an A.I. platform can help with.
And because we are still in the early stages of A.I. adoption, there is an opportunity to introduce these tools in a vendor-neutral, teaching environment. So we can show the A.I. technology to a hospital, and say, “Here are the possibilities of what you could do with this. Here’s how it works. And here are the opportunities and challenges.” RAD-AID can be the partner to that low-resource hospital to help navigate the application of A.I. in clinical care.

Dr. Allison Borowski, RAD-AID Volunteer, helping breast imaging in support of radiology residency training and breast cancer screening in Guyana.
Mo: So, essentially what you’re saying is that while there’s a real potential for A.I. tools to improve care in low-resource regions that typically do not have access to such technologies, it is important that these technologies be introduced with care.
Dan: That’s right. If we consider again the case of Kenya, where there’s 4-5 million women in need of mammography, and you only have a handful of breast radiologists available to read those images, then it raises the question of whether an A.I. platform for mammography, whether it’s for quality control or for interpretation, could somehow impact that workflow to empower the radiologist to do a more effective job with such a large screening population.
Those are the kinds of questions that A.I. can potentially answer, and really needs a first introduction to explore what those possibilities might be.
9. Mo: From your experience, do you think these under-resourced regions are receptive to the use of A.I.? Do they have the same hesitations that we see in the current discourse around A.I. in well-resourced areas?
Dan: That’s a great question because most of the dialogue on A.I. is focused on the adoption of A.I. in the high-income region setting, where there is an assumption that you have an abundant labour supply, and an abundant medical imaging equipment supply. Therefore you are putting A.I. into a well-resourced context where there is an experienced radiologist to interpret the output, and they can evaluate that output in the context of what they know from their own clinical experience.
In contrast to that, the low-income country setting may not have any radiologists, and may not have anyone with sufficient experience to interpret the A.I. outputs. Who’s going to know if the A.I. output is correct or have confidence in being able to use the results to make a clinical decision? So that requires a real collaboration between the low-resource hospital and RAD-AID through educational resources to help these hospitals to engage effectively with A.I., and implement it safely.
The A.I. knowledge gap between high-income and low-income countries is substantial.
10. Mo: What kind of outcomes does RAD-AID hope to achieve from partnering with Densitas?
Dan: The ultimate outcomes we are working towards are improved breast cancer screening through earlier detection which then leads to better treatment and saving lives. A collaboration with Densitas presents the opportunity of applying Densitas A.I. technologies to deliver better care in low-income countries and medically underserved regions, supporting radiologists and radiological technologists to deliver precision breast health with a special focus on clinical image quality.
Let’s Stay Connected, Subscribe for Updates
Join our email list to stay up to date on the latest advancements in breast health technology.
Sign Me Up
 USA
USA UK
UK Canada
Canada